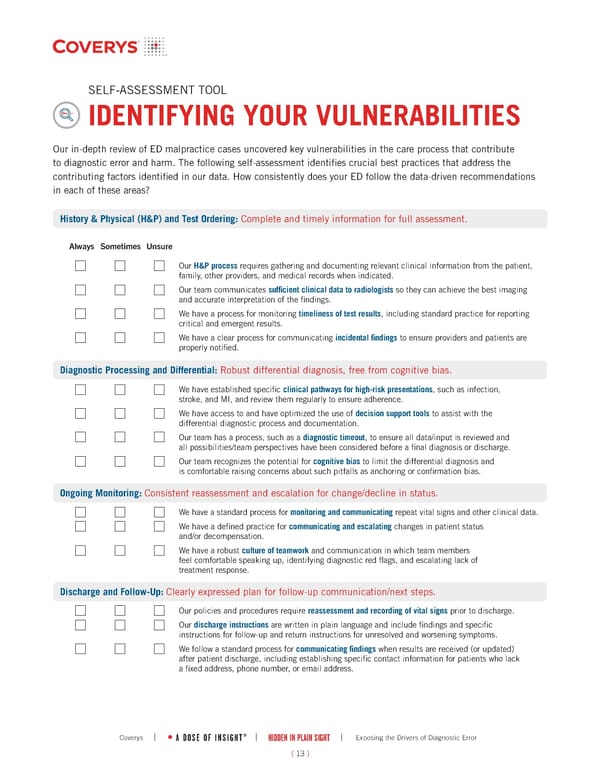
SELF-ASSESSMENT TOOL IDENTIFYING YOUR VULNERABILITIES Our in-depth review of ED malpractice cases uncovered key vulnerabilities in the care process that contribute to diagnostic error and harm. The following self-assessment identifies crucial best practices that address the contributing factors identified in our data. How consistently does your ED follow the data-driven recommendations in each of these areas? ( 13 ) Diagnostic Processing and Differential: Robust differential diagnosis, free from cognitive bias. History & Physical (H&P) and Test Ordering: Complete and timely information for full assessment. Our H&P process requires gathering and documenting relevant clinical information from the patient, family, other providers, and medical records when indicated. Our team communicates sufficient clinical data to radiologists so they can achieve the best imaging and accurate interpretation of the findings. We have a process for monitoring timeliness of test results, including standard practice for reporting critical and emergent results. We have a clear process for communicating incidental findings to ensure providers and patients are properly notified. Always Sometimes Unsure We have established specific clinical pathways for high-risk presentations, such as infection, stroke, and MI, and review them regularly to ensure adherence. We have access to and have optimized the use of decision support tools to assist with the differential diagnostic process and documentation. Our team has a process, such as a diagnostic timeout, to ensure all data/input is reviewed and all possibilities/team perspectives have been considered before a final diagnosis or discharge. Our team recognizes the potential for cognitive bias to limit the differential diagnosis and is comfortable raising concerns about such pitfalls as anchoring or confirmation bias. Ongoing Monitoring: Consistent reassessment and escalation for change/decline in status. We have a standard process for monitoring and communicating repeat vital signs and other clinical data. We have a defined practice for communicating and escalating changes in patient status and/or decompensation. We have a robust culture of teamwork and communication in which team members feel comfortable speaking up, identifying diagnostic red flags, and escalating lack of treatment response. Discharge and Follow-Up: Clearly expressed plan for follow-up communication/next steps. Our policies and procedures require reassessment and recording of vital signs prior to discharge. Our discharge instructions are written in plain language and include findings and specific instructions for follow-up and return instructions for unresolved and worsening symptoms. We follow a standard process for communicating findings when results are received (or updated) after patient discharge, including establishing specific contact information for patients who lack a fixed address, phone number, or email address. | HIDDEN IN PLAIN SIGHT | Exposing the Drivers of Diagnostic Error A DOSE OF INSIGHT ® Coverys |
 Hidden in Plain Sight: Exposing the Drivers of Diagnostic Error Page 13 Page 15
Hidden in Plain Sight: Exposing the Drivers of Diagnostic Error Page 13 Page 15