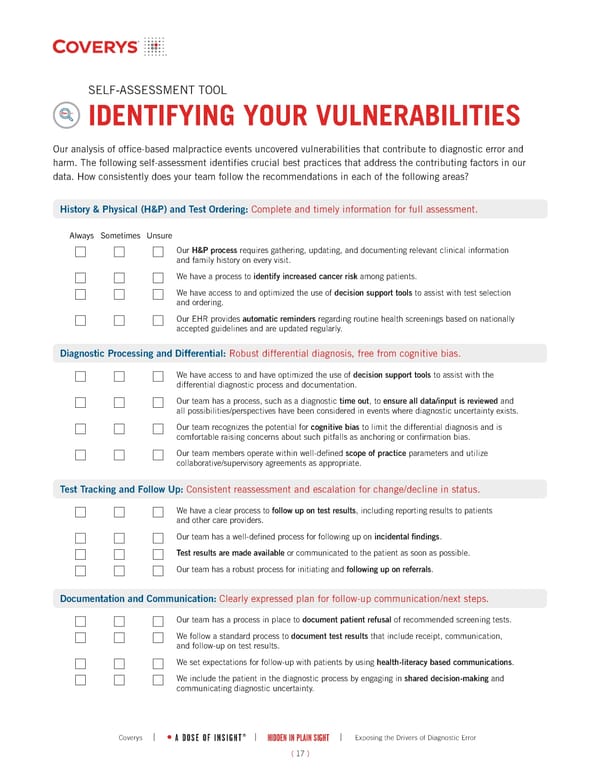
( 17 ) | HIDDEN IN PLAIN SIGHT | Exposing the Drivers of Diagnostic Error A DOSE OF INSIGHT ® Coverys | SELF-ASSESSMENT TOOL IDENTIFYING YOUR VULNERABILITIES Our analysis of office-based malpractice events uncovered vulnerabilities that contribute to diagnostic error and harm. The following self-assessment identifies crucial best practices that address the contributing factors in our data. How consistently does your team follow the recommendations in each of the following areas? Diagnostic Processing and Differential: Robust differential diagnosis, free from cognitive bias. History & Physical (H&P) and Test Ordering: Complete and timely information for full assessment. Our H&P process requires gathering, updating, and documenting relevant clinical information and family history on every visit. We have a process to identify increased cancer risk among patients. We have access to and optimized the use of decision support tools to assist with test selection and ordering. Our EHR provides automatic reminders regarding routine health screenings based on nationally accepted guidelines and are updated regularly. Always Sometimes Unsure Test Tracking and Follow Up: Consistent reassessment and escalation for change/decline in status. We have a clear process to follow up on test results, including reporting results to patients and other care providers. Our team has a well-defined process for following up on incidental findings. Test results are made available or communicated to the patient as soon as possible. Our team has a robust process for initiating and following up on referrals. Documentation and Communication: Clearly expressed plan for follow-up communication/next steps. Our team has a process in place to document patient refusal of recommended screening tests. We follow a standard process to document test results that include receipt, communication, and follow-up on test results. We set expectations for follow-up with patients by using health-literacy based communications. We include the patient in the diagnostic process by engaging in shared decision-making and communicating diagnostic uncertainty. We have access to and have optimized the use of decision support tools to assist with the differential diagnostic process and documentation. Our team has a process, such as a diagnostic time out, to ensure all data/input is reviewed and all possibilities/perspectives have been considered in events where diagnostic uncertainty exists. Our team recognizes the potential for cognitive bias to limit the differential diagnosis and is comfortable raising concerns about such pitfalls as anchoring or confirmation bias. Our team members operate within well-defined scope of practice parameters and utilize collaborative/supervisory agreements as appropriate.
 Hidden in Plain Sight: Exposing the Drivers of Diagnostic Error - PART II Page 17 Page 19
Hidden in Plain Sight: Exposing the Drivers of Diagnostic Error - PART II Page 17 Page 19